What Is Palliative Care?
Understanding Hospice Care in the UK

If someone you love has received a serious diagnosis, you might be hearing terms like “palliative care” and “hospice care” for the first time. It’s completely normal to feel uncertain about what these words actually mean – which is exactly why we’ve written this guide to help.
When we don’t understand something, our minds often fill in the gaps with assumptions. And when it comes to palliative care and hospices, those assumptions are frequently wrong. Many people picture hushed rooms and final goodbyes. The reality couldn’t be more different.
What does palliative care actually mean?
Palliative care is specialist medical care focused on providing relief from the symptoms, pain and stress of a serious illness. The goal is straightforward: to improve quality of life for both the patient and their family.
Here’s the important bit that surprises many people – palliative care isn’t just for the end of life. It can begin at any point after a serious diagnosis and can be provided alongside curative treatment. Someone receiving chemotherapy, for instance, might also receive palliative care to help manage side effects and maintain their wellbeing.
The World Health Organization describes palliative care as an approach that improves quality of life for patients and families facing challenges associated with life-limiting illness. It’s about living as well as possible, for as long as possible.
Palliative care and hospice care – what's the difference?
This is where things can get a bit confusing, so let’s untangle it.
Palliative care is a broad approach to care that can be delivered in many settings: hospitals, GP surgeries, care homes, or someone’s own home. Hospice care is a form of palliative care, typically provided by specialist hospice organisations.
Hospices in the UK offer far more than most people realise. They provide expert medical care, certainly, but also emotional support, practical help, and specialist therapies. They support families and carers too, during illness and through bereavement.
And crucially, hospice care happens wherever it’s needed. You might be surprised to know that only around a fifth of hospice care actually takes place in hospice inpatient units. In fact, more than half of all hospice care took place in patients’ own homes.
The numbers tell an important story
Understanding the scale of palliative care need in the UK helps put things in perspective.
Research suggests that around 90% of people who die in the UK could benefit from palliative care. That’s not a small number of people at the margins – it’s almost everyone.
In 2024-25, hospices across the UK provided palliative and end of life care to 310,000 people. They made 590,000 home visits by specialist palliative care nurses and doctors, provided 610,000 days and nights of inpatient care, and offered 470,000 appointments to patients’ families for counselling and bereavement support.
There are around 170 adult hospices and 40 children’s hospices in England. Yet despite this network of care, the proportion of people dying in hospital remains significant – 42% in 2024. Only 5% of deaths occurred in hospice inpatient units, whilst 28% happened at home and 21% in care homes.
These figures point to something important: there’s a gap between the care people need and the care that’s currently available.
Busting the myths about hospice care
Let’s tackle some common misconceptions head-on.
1. “You only go to a hospice to die.”
This is perhaps the most persistent myth, and it simply isn’t true. Many hospice patients are admitted for short stays – perhaps for pain management, symptom control, or to give their carers a much-needed break. Around 40-50% of people admitted to hospice inpatient units return home afterwards.
Hospices support people at various stages of illness, sometimes for years. It’s about living well, not just dying well.
2. “Hospices are sad, depressing places.”
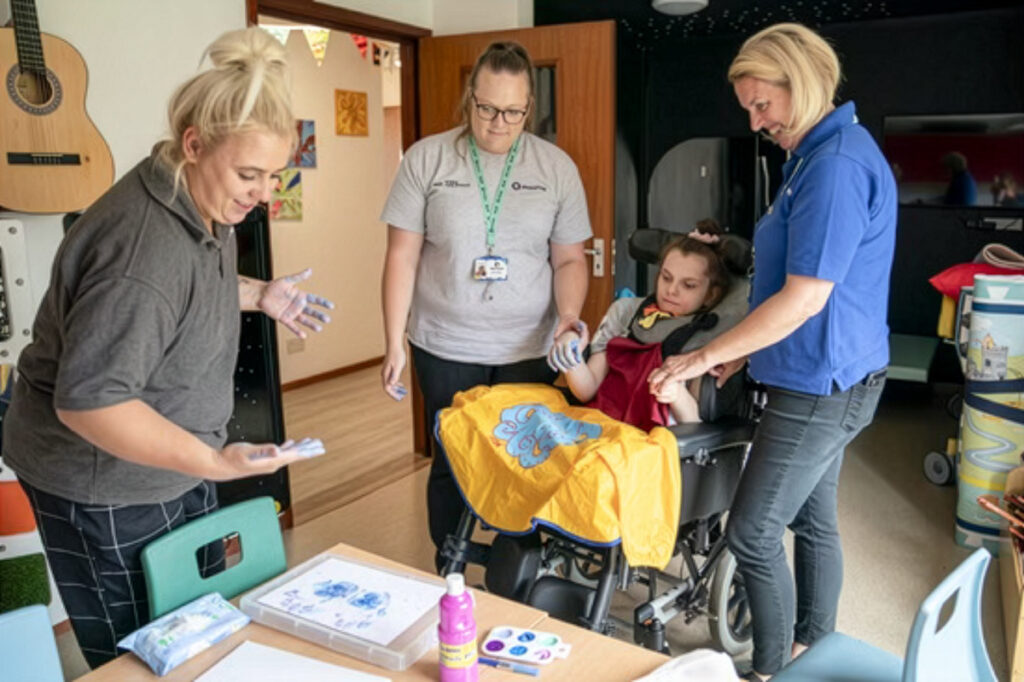
Walk through the doors of most hospices and you’ll find warmth, colour, and yes – laughter. Staff consistently describe hospices as positive working environments. Patients and families often speak of feeling welcomed, supported, and cared for in ways that simply aren’t possible in busy hospital wards.
There are difficult moments, of course. But hospices create space for connection, for memory-making, and for quality time together.
3. “Hospice care is only for people with cancer.”
While cancer patients do make up a significant proportion of those receiving hospice care, hospices support people with many different conditions. Heart failure, respiratory disease, motor neurone disease, kidney disease, Parkinson’s, and other neurological and genetic conditions – hospices provide specialist care for all of these and more.
If you have a life-limiting illness of any kind, hospice care may be available to you.
4. “It’s only for older people.”
Hospice care is available to adults of all ages. In fact, around 25% of people who die in UK hospices are under 65. There are also specialist children’s hospices providing care for young people and their families.
5. “Once you’re in a hospice, you can’t leave.”
Patients have complete choice about their care. Many people move between home, hospital and hospice depending on their needs at different times. Hospice care is flexible and responsive – it adapts to whatever each person needs.
How hospices are funded
Something that surprises many people is how hospices pay for their services.
Most hospices in the UK are independent charities. They receive only around one-third of their funding from the NHS, with the remainder coming from charitable donations, fundraising, legacy gifts, and their own shops and lotteries.
This means that the compassionate, specialist care provided by hospices depends significantly on community support. Every donation, every sponsored walk, every gift in a will – these contributions directly enable hospices to continue their work.
The UK Government announced a £100 million capital investment for hospices in late 2024, alongside £26 million revenue funding for children’s hospices.
This was welcome news – BUT capital funding can only be spent on buildings and equipment, not on staff wages or day-to-day running costs. With rising costs and increased employer National Insurance contributions, many hospices remain under significant financial pressure.
The need for community support has never been greater.
What happens in hospice care?
Hospice care addresses what professionals call the “whole person” – physical, emotional, social and spiritual needs.
On the physical side, hospice teams are experts in pain management and symptom control. They can often achieve comfort that has proved difficult elsewhere, helping people feel more like themselves again.
But physical care is just one part. Hospices offer counselling, complementary therapies like massage and aromatherapy, physiotherapy, occupational therapy, and chaplaincy support for those who want it. They help with practical matters too – benefits advice, family support, and help navigating the healthcare system.
For families and carers, hospices provide respite, emotional support, and guidance through what can be an overwhelming time. Bereavement support continues after a death, for as long as it’s needed.
The growing need for palliative care
Here’s something we all need to understand: the demand for palliative and end of life care is rising, and it will continue to rise.
Our population is ageing. The number of people aged 85 and over is projected to more than double in some parts of the UK over the next 25 years. Research suggests a 25% increase in palliative care need by 2048.
This isn’t a distant problem. It’s happening now, and it affects us all – either directly or through the people we love.
Supporting hospices and palliative care services isn’t just about helping strangers. It’s about ensuring that when our time comes, or our parents’ time, or our friends’ time, the care that makes such a profound difference will still be there.
How you can help
There are many ways to support hospice care in the UK.
Donating to charities like Hospice Aid UK helps ensure hospices can continue providing their vital services. Regular giving, however small, allows organisations to plan ahead and sustain their work.
Fundraising – whether running a marathon, organising a coffee morning, or taking part in a sponsored challenge – brings communities together whilst raising essential funds.
Leaving a gift in your will is one of the most powerful ways to support hospice care for future generations. Many people don’t realise that legacy gifts form a significant part of hospice funding.
And simply talking about hospice care helps too. Sharing your own experiences, recommending that others look into hospice support, challenging the myths when you hear them – all of this makes a difference.
Finding hospice care
If you or someone you love might benefit from hospice care, the first step is usually a conversation with your GP or hospital consultant, who can make a referral.
You can also contact your local hospice directly – most have information teams who can explain what services are available and how to access them.
Remember, you don’t have to wait until a crisis point. Hospice care can help from the point of diagnosis, supporting you to live as well as possible throughout your illness.
About Hospice Aid UK
Hospice Aid UK supports hospices across the UK and Northern Ireland to provide exceptional end of life and respite care. Find out how you can help.
Share this post: Help us reach more people who want to support hospice care by sharing our blog post online.
